Think fungal infections are just annoying skin irritations like athlete’s foot and jock itch? Think again. The rise of antifungal resistance means the game has changed. What was once a surefire treatment is now uncertain, and severe, life-threatening fungal diseases are on the rise.
Published May 22, 2024

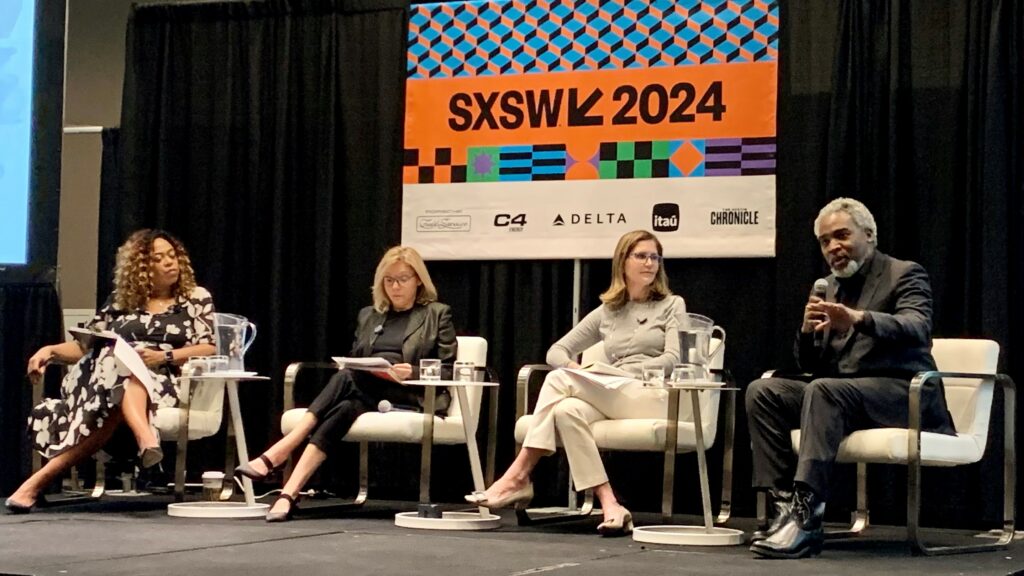
Fungi are everywhere: in the soil, on our skin, and in the air we breathe. They give us the cheese on our burgers and the beer and wine we love. Despite their benefits, fungi aren’t always our friends. Every day, we inhale up to 100,000 or more fungal spores—our immune system usually keeps infections at bay. Yet, out of the estimated 2-11 million fungal species, about 200 can make us sick. On March 11, 2024, the South by Southwest Conference panel “Will Fungi Be the Last of Us?,” moderated by public health journalist and author Maryn McKenna, explored how fighting harmful fungal species is a growing public health challenge.
The Agricultural Connection: How Fungicides Fuel Drug Resistance
While we may inhale numerous fungi, our primary defense against fungal infections is our body temperature—most fungi can’t survive the heat of our lungs and prefer cooler environments. However, certain fungal species like Candida auris and Aspergillus thrive at human body temperature and can cause severe disease in hospitalized patients with weakened immune systems. Panelist Paul Verweij, MD, FECMM, Professor of Clinical Mycology at Radboud University Medical Center of Expertise for Mycology, highlighted the threat of Candida auris: “This is a new yeast, which is emerging, and has spread all over the world since 1996. One of the problems with (it) is that it is drug resistant.”
Dr. Verweij explained that exposure to agricultural azoles, chemical fungicides used on food crops, has driven this fungus to develop resistance to azoles. “The problem we face in hospitals is that we use the same type of drugs to treat our patients,” Verweij lamented.
The panel highlighted the urgent need for a comprehensive approach to the development of agricultural fungicides that do not have harmful ramifications for human health. Panelist John Rex, MD, FACP, Chief Medical Officer at the antifungal biotech F2G, Ltd., cited a 2023 concept paper issued by the US Environmental Protection Agency and developed in collaboration with the US Department of Health and Human Services, the US Department of Agriculture, and offices within the White House Executive Office of the President.
The paper, titled Concept for a Framework to Assess the Risk to the Effectiveness of Human and Animal Drugs Posed by Certain Antibacterial or Antifungal Pesticides, sought public feedback on potential solutions, research, or mitigation approaches to reduce the spread of antimicrobial resistance (AMR). Panelist Tom Chiller, MD, MPHTM, Chief of the Mycotic Diseases Branch at the Centers for Disease Control and Prevention added, “The key is that we’re bringing groups together that don’t traditionally talk. We need to recognize that we each have problems that are going to be solved with these medicines. But how do we do it together so that we don’t affect that critical treatment [for a] patient with a fungal disease?”
Rising Temperatures, Rising Threats: Fungi in a Changing Climate
Dr. Chiller also emphasized the impact of climate change on the evolution of fungal species. “Fungi live out in the environment. If the environment changes—and climate change is causing environmental changes—the fungi have to adapt. They are going to try to tolerate higher temperatures. We need to understand that more.” Chiller pointed to Valley Fever, caused by the soil-based fungus Coccidioides: “It’s mainly in the Southwest [of the US], but now we know that the geographic area of this fungus is spreading. I have to think that climate change is playing a role.”
Closer Cousins Than You Think
Dr. Rex highlighted a critical difference in treating bacterial versus fungal infections. “You’ve heard of things like penicillin, sulfa [drugs], and erythromycin. There are at least a dozen completely different kinds of treatments for bacterial infections.” In contrast, Rex noted, “for fungi, there are only three major classes. The reason …. is that, believe it or not, one of your closest cousins is the fungi. We’re quite closely related, genetically. To find something that just kills the fungus and not the person, that’s hard. There are very few novel classes [of antifungal drugs] and each one we find is a precious jewel.”
Rapid diagnosis of fungal infection also remains challenging. Patient symptoms are often non-specific, and the sensitivity and specificity of available tests vary widely. Dr. Verweij shared his clinical experiences: “With only two classes of drug treatment available for Aspergillus infection, resistance to one treatment leaves the physician with just one drug to administer to the patient.” He highlighted the severe toxic side effects and the limited reach of these drugs. “If the infection spreads from the lung to the brain, then it’s extremely difficult to treat, and you can end up with an untreatable infection.”
Reviving Antimicrobial Development: The Promise of the PASTEUR Act
“Over the past decade, we’ve had several new antibiotics get approved, and then the companies go bankrupt,” Dr. Rex noted. He emphasized the importance of creating a sustainable financial model for developing and distributing new antimicrobials. “I’m very concerned that the ecosystem of people who know how to invent these drugs is drying up,” he warned. Dr. Rex shared his 15-year involvement in the development of the Pioneering Antimicrobial Subscriptions To End Upsurging Resistance Act of 2023 (PASTEUR Act).
This bill, re-introduced in the US Senate in April 2023, aims to stimulate innovative drug development, improve the appropriate use of antibiotics, and ensure domestic availability of critical need antimicrobial medicines to prevent AMR from becoming the next global pandemic. The PASTEUR Act proposes an innovative payment model where the US federal government invests $6 billion over 10 years in novel antibiotics and antifungals through installment payments. In return, developers would provide their drugs free of charge to government programs once available. This initiative is designed to foster much-needed investment and prepare the nation’s health care system for the increasing threat of antibiotic- and antifungal-resistant infections.
Antifungal Development in the AI Era
Conference discussion also centered on the pervasive influence of artificial intelligence (AI) across diverse industries and its role in antifungal development naturally emerged. Dr. Rex emphasized the immense potential of AI tools in assessing the toxicity risks associated with promising molecules identified during drug development. He noted, “That has, so far, evaded all simple prediction tools.”
Learn more about the dual nature of fungi—beneficial allies and deadly foes—at the July 18, 2024 hybrid Academy event featuring a conversation with mycologist, immunologist, and author Arturo Casadevall, MD, PhD, about his new book, What if Fungi Win?